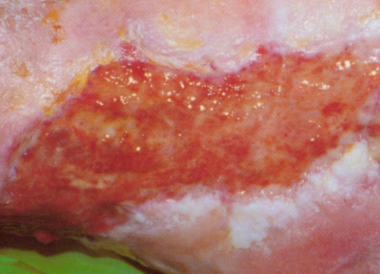
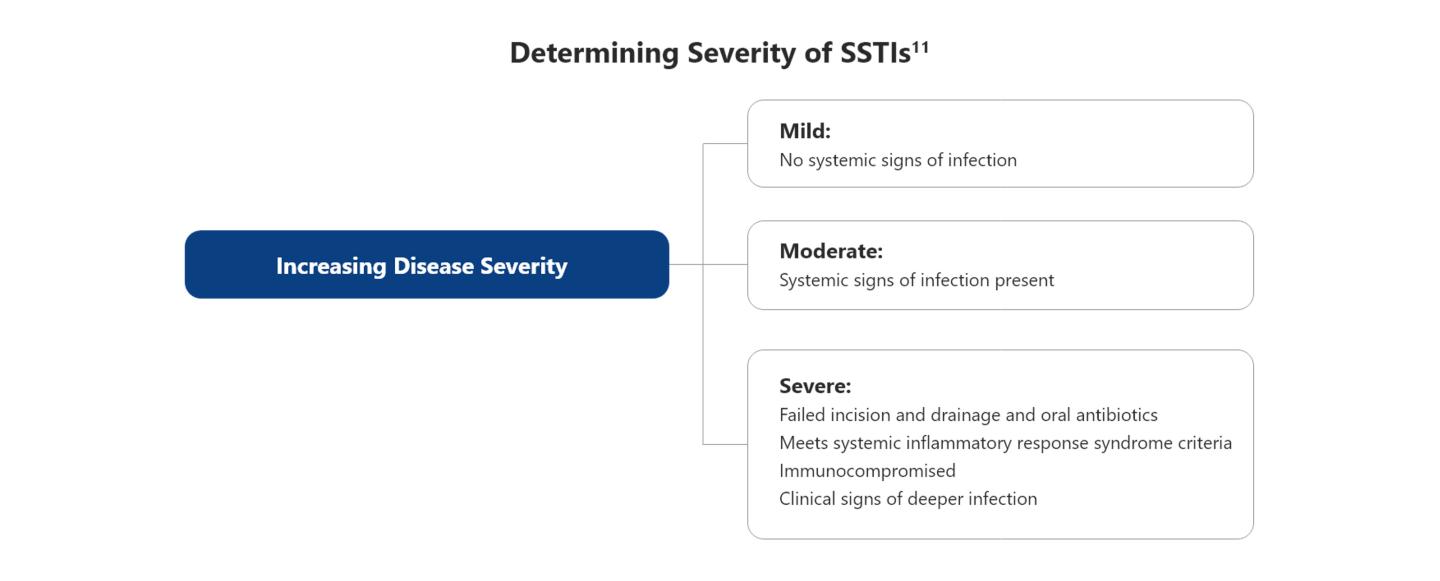
Comprehensive diagnosis of SSTIs often starts with a clinical history and findings from physical examination that help assess the severity of an infection. Although diagnosis of SSTIs is based on clinical presentation, microbiologic investigation is recommended in certain situations; for example, routine Gram-stain and culture of purulent material from carbuncles and abscesses are recommended by the Infectious Disease Society of America (IDSA).11 A precise diagnosis guides the decision on prompt and appropriate treatment.3,11
Radiological examination and imaging aid investigations of deep tissue infections to assess site and size of infection and any vascular involvement which can guide surgical drainage procedures.1,3 For patients with severe infection or comorbid conditions, common laboratory investigations can include complete blood count, C-reactive protein level, and liver and kidney function tests.1,3
Diagnosis of SSTIs relies primarily on clinical examination and findings, although microbiological investigation confirms the cause in over 60% of cases, suggesting a predominance of Gram-positive bacteria.2 The approach to diagnosis should follow the principles set out in guidelines from the Infectious Diseases Society of America (IDSA) on SSTIs, which involves assessment of severity, and recommends management approaches based on whether infections are purulent or non-purulent.