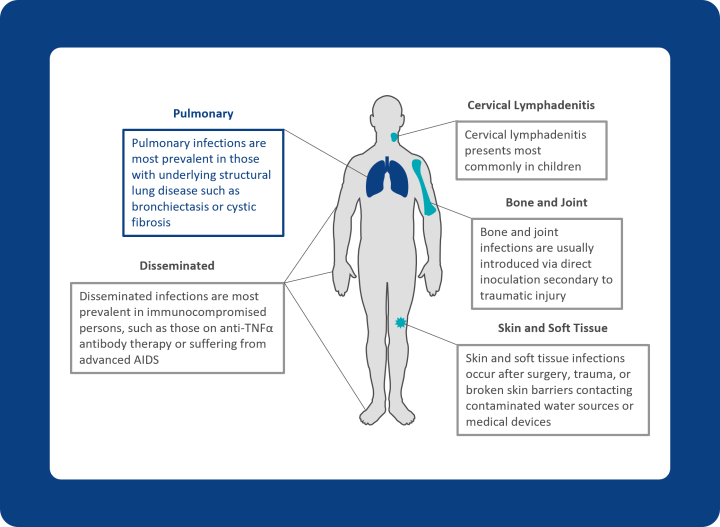
NTM pulmonary disease is a slowly progressing, chronic disease, often with debilitating outcomes. It disproportionately impacts individuals over 45 years of age, particularly those with preexisting structural lung disease, as well as younger patients with cystic fibrosis.2
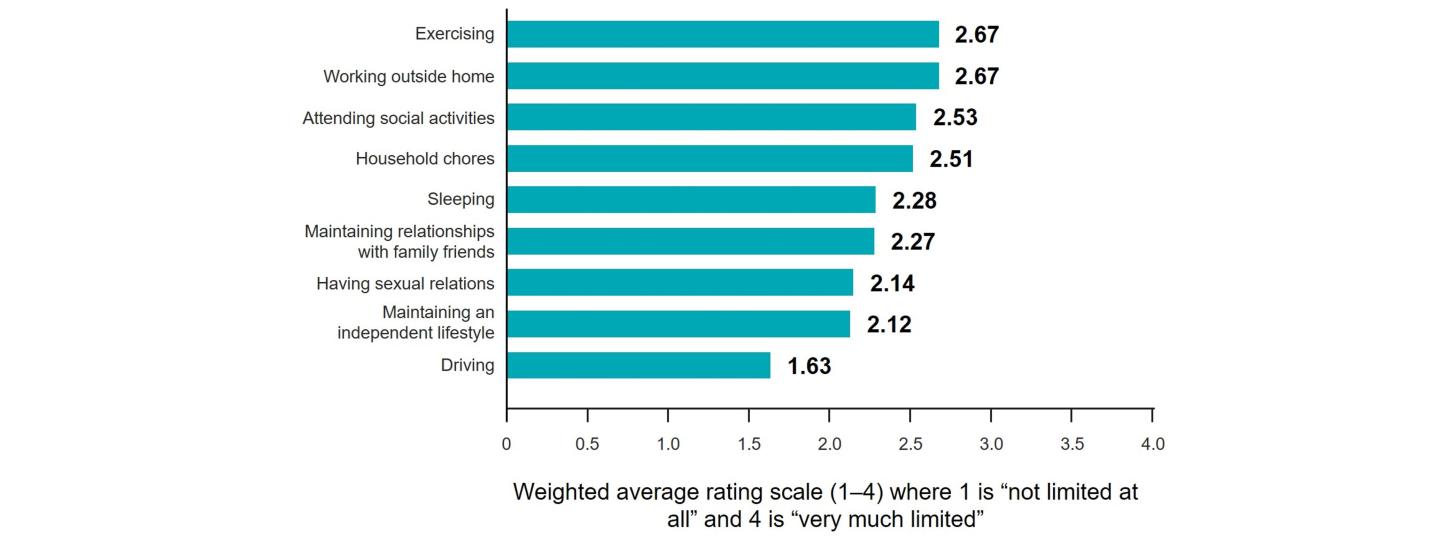
NTM pulmonary disease is associated with decreased respiratory function over time and patients often have significantly impaired quality of life, experiencing limitations to several daily activities, as shown below.3,8 The condition is also associated with increased morbidity and mortality rates; when compared with a matched control group and followed for ~3.5 years, all-cause mortality rates were more than double in patients with NTM pulmonary disease.9