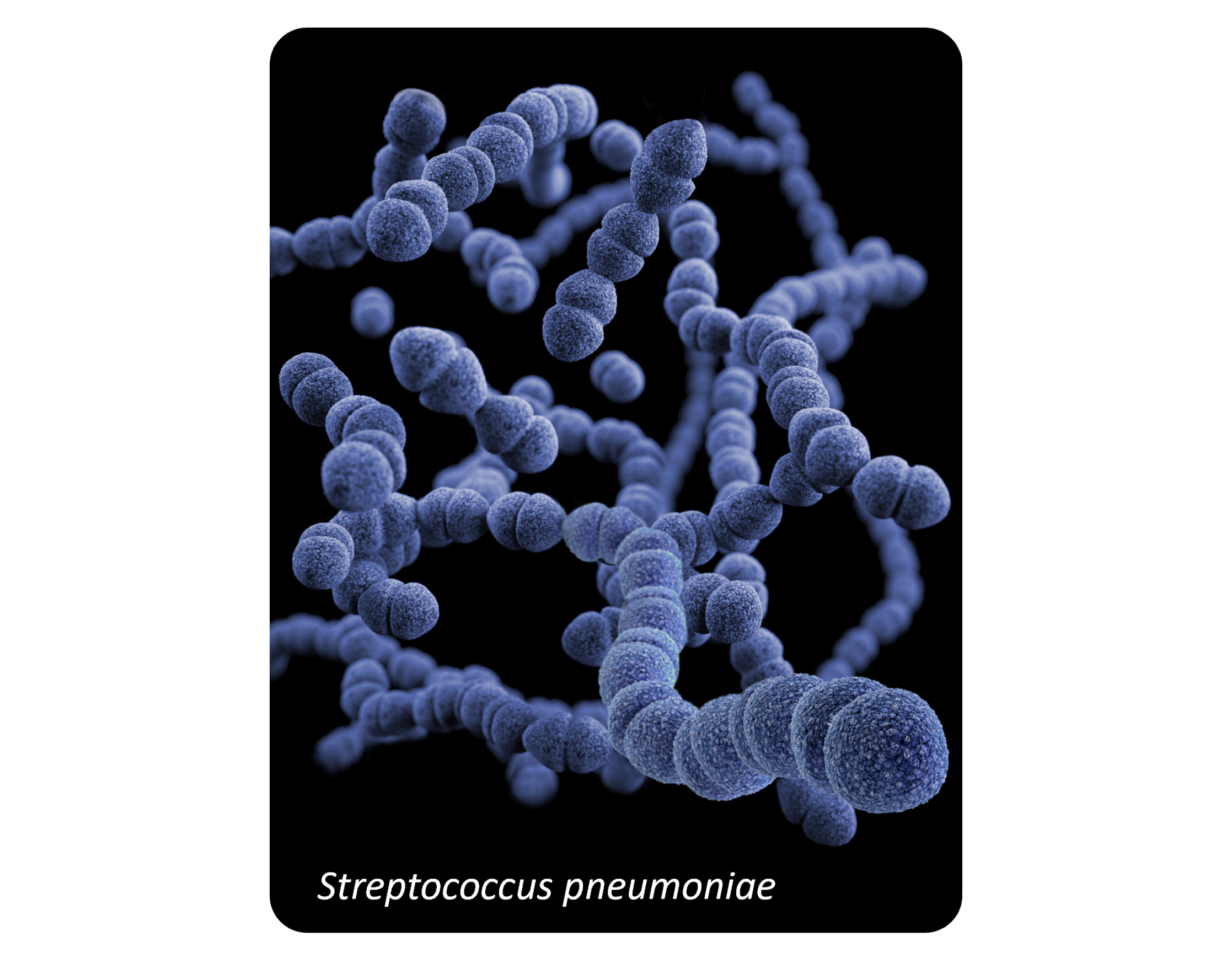
Streptococcus pneumoniae is the most commonly identified cause of CAP, still implicated in 5–15% of cases requiring hospitalization in the US, despite declining in frequency.1,2
Drug-resistant Streptococcus pneumoniae has been classified by CDC as a serious threat based on the current rates of resistance to commonly used antibiotics.3
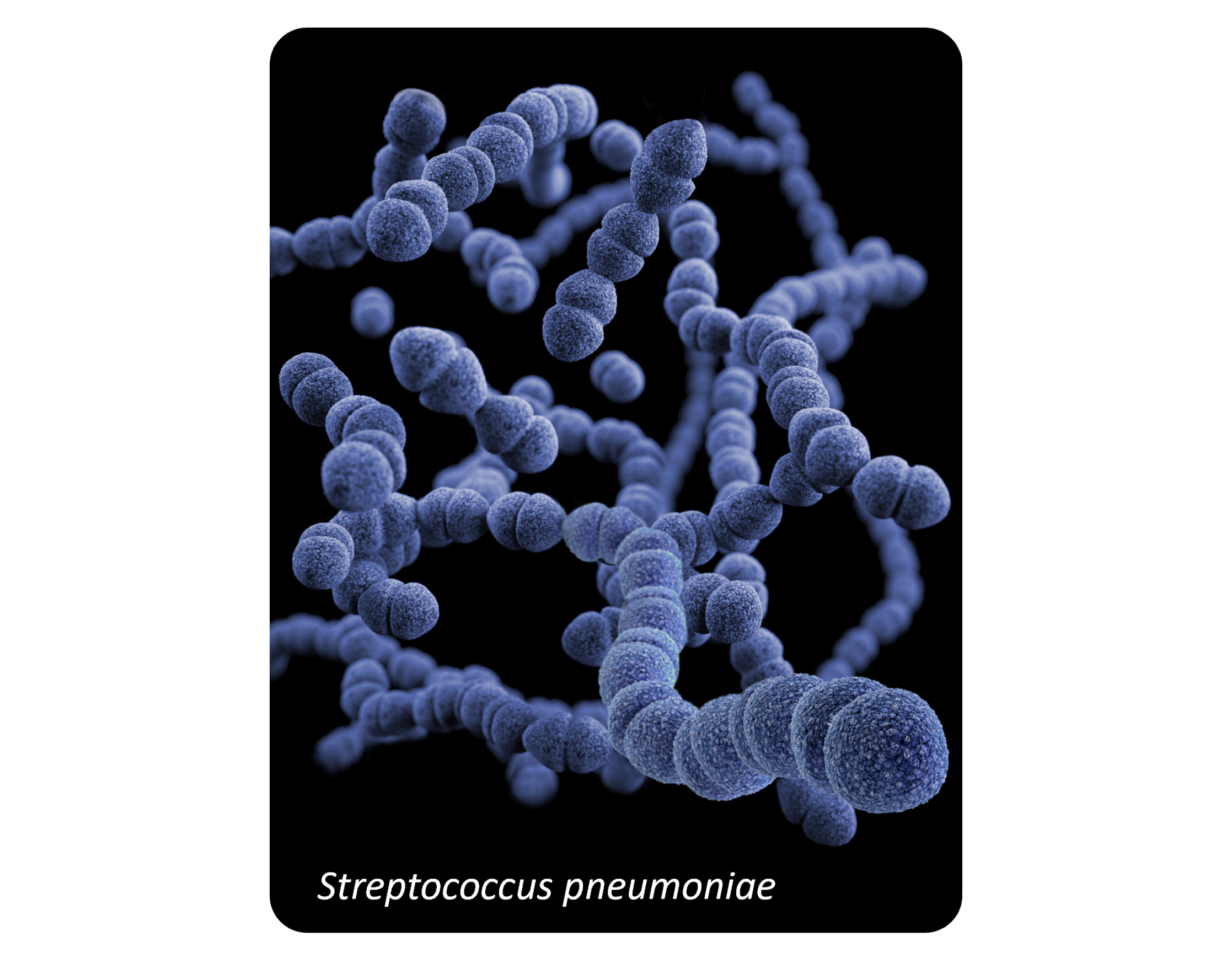
This illustration depicts a three-dimensional (3D), computer-generated image, of a group of Gram-positive, Streptococcus pneumoniae bacteria. The artistic recreation was based upon scanning electron microscopic (SEM) imagery. Image courtesy of the Antibiotic Resistance Coordination and Strategy Unit - Medical Illustrator, via the Public Health Image Library of the Centers for Disease Control and Prevention.
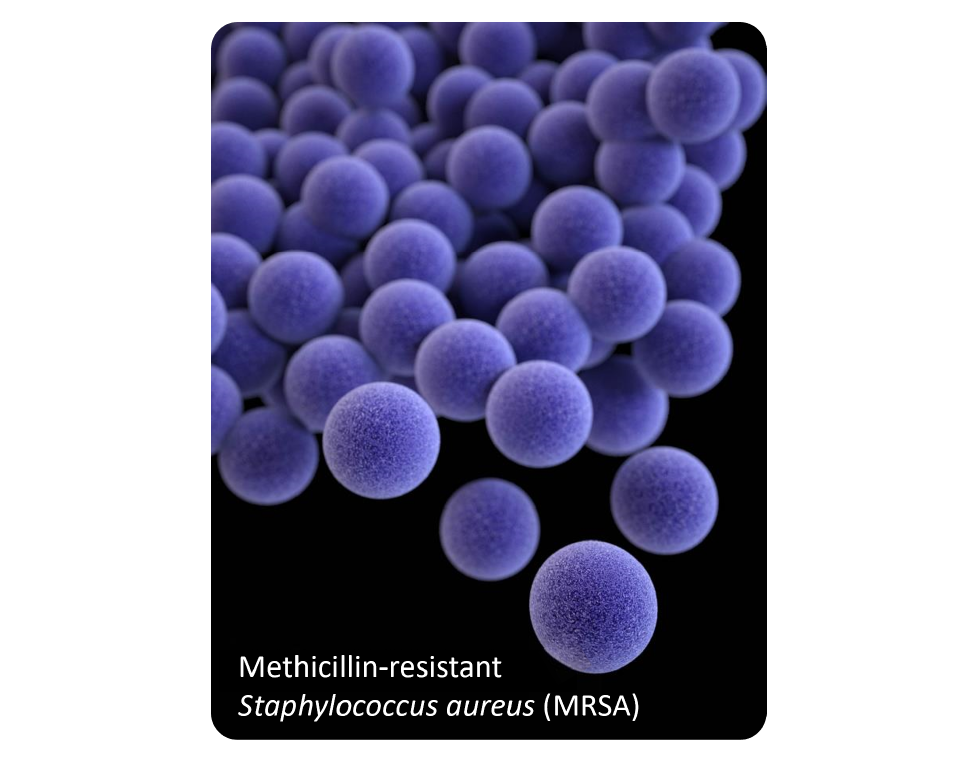
Staphylococcus aureus is an important cause of CAP. Methicillin-resistant Staphylococcus aureus (MRSA) can occur in the setting of recent or concurrent influenza infection and may cause severe disease in previously healthy patients.4
This illustration depicts a three-dimensional (3D) computer-generated image of a group of methicillin-resistant Staphylococcus aureus (MRSA) bacteria, which were arranged in a cluster. The artistic recreation was based upon scanning electron microscopic (SEM) imagery. Image courtesy of the Antibiotic Resistance Coordination and Strategy Unit - Medical Illustrator, via the Public Health Image Library of the Centers for Disease Control and Prevention.